Lawmakers tear into Ohio Medicaid officials: Are you incompetent?
Enraged by pharmacy middlemen making millions on Ohio’s health insurance program for the poor and disabled, lawmakers tore into Medicaid officials Thursday, accusing them of withholding data, failing to recognize the scope of the problem, and ignoring recommendations for reducing costs.
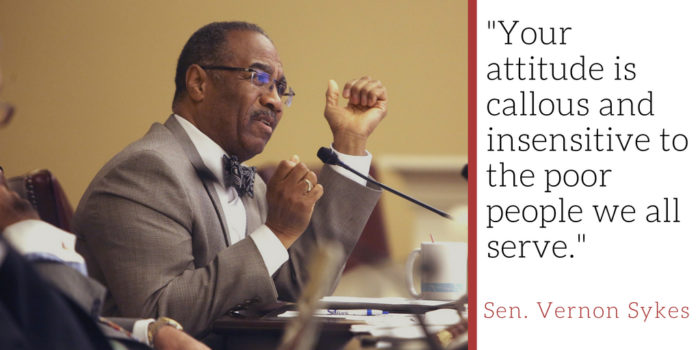
"Your attitude is callous and insensitive to the poor people we all serve," said Sen. Vernon Sykes, D-Akron, as he scolded Medicaid officials before the Joint Medicaid Oversight Committee.
Sykes, one of the legislature's longest-serving lawmakers, pulled no punches, surprising those who know his usual soft-spoken temperament.
"We’re talking about hundreds of millions of dollars, and I sit here as a senator that represents a lot of poor people. ... They just can’t even imagine how much money this is. And for you to stand here with a straight face, and say you don’t think this is a crisis. With a straight face, you say you don’t think there is any need for any immediate regulatory intervention. With a straight face, you say you’re going to ask the providers do they think that maybe they can come up with a better deal, and if we can, then maybe we might implement it.
“You’ve sworn several times to be a good steward of public assets, resources. But the system is controlled by you, designed by you and operated. So it is incompetent. The question that I really have is whether or not you are incompetent."
Patrick Stephan, director of managed care for Medicaid, said he didn’t mean to appear insensitive. “I will apologize to all the members of this committee if my presentation style was offensive. That was not my intent … we will continue to look into this to get to a resolution.”
Medicaid officials were brought before JMOC to discuss a report commissioned by the state that found pharmacy benefit managers, or PBMs, billed taxpayers $223.7 million more for prescription drugs in a year than they reimbursed pharmacies to fill those prescriptions.
That 8.8 percent difference, known as the price spread, represents millions kept by CVS Caremark and Optum Rx, PBMs for Ohio Medicaid’s five managed care plans. Largely pass-through operations, PBMs negotiate drug prices with manufacturers and process drug claims.

The study, conducted by Columbus consultant HealthPlan Data Solutions, said PBM fees should be in the range of 90 cents to $1.90 per prescription. CVS Caremark billed the state about $5.60 per script; Optum charged $6.50 — three to six times higher. But Medicaid officials didn't even mention those figures from the report, which they are withholding from the public (only an executive summary has been revealed).
Earlier, Stephan told lawmakers, “we concluded there is not necessarily justification for a crisis and immediate regulatory intervention. However, we understand that there is always room for improvement.”
“We believe the price transparency we have now sets us up to get a better deal” when contracts with the managed care plans that hire PBMs.
Medicaid Director Barbara Sears told the panel that PBMs were not the problem: “High drug prices begin with drug manufacturers.”
Asked about Sears' claim, PhRMA spokesman Nick McGee said in an e-mail, "We welcome the opportunity to work with Ohio Medicaid to look across the supply chain to help ensure patients can access and afford their medicines."
Lawmakers said they think payments to PBMs are excessive and want a better deal now. Price spread, they said, is just a part of the equation.
Sen. William Coley, R-West Chester, said the $223.7 million paid to PBMs cited in the report is low, because it does not include all drug rebates from manufacturers, pharmacy rebates and transaction fees collected by PBMs. Coley said he calculated the PBMs earnings to be at least $516 million — more than one-fifth Ohio's Medicaid's drug spend — and that doesn't include specialty drug revenues, information that was not provided to lawmakers.
"Five-hundred-something million? Think about that, and that's what we know about," Coley said.
Sen. Lou Terhar, R-Cincinnati, said the system creates incentives for PBMs like CVS Caremark, which handles most Medicaid prescriptions, to dispense as many drugs as possible.
“My observation is if the PBM is the one who buys the drugs and also has outlets to sell the drugs, that if I’m that person and I know I’m getting rebates on volume, do I really care how much my pharmacies make? … The spread between what independent pharmacies get and what they get is not really the issue. The issue is how much money do they get back in rebates, which could be two or three times that number … they can control the prices at the bottom because the money is coming in at the top.
“If you get more money in rebates it is in your interest to push more drugs out, not less. Is that really what we’re trying to do?”
Rep. Mark Romanchuk, R-Mansfield, told Medicaid officials, "rest assured, with the administration’s help we’re going to make this better.”
He asked if they still believe $5.70, the state’s average per-prescription cost charged by the PBMs, was “reasonable.”
Sears called it “in the ballpark. I don’t think we’ve decided if it can be improved or not.”
Romanchuk noted that Meridian Rx, a PBM not involved in Ohio’s Medicaid program, told The Dispatch it charges Medicaid clients about $2 per prescription.
“Based on that information does $5.70 still look very reasonable?” he wanted to know.
“On the surface the most rational people would say no,” Stephan said, adding he’d need more information on what that cost included. “We should be able to get a better deal with transparency."
Lawmakers also complained that they were given only a summary of the report. Medicaid said they cannot release it because it “contains information that may be proprietary and, or, contain trade secrets.”