SIDE EFFECTS
An ongoing investigation on the rising costs of prescription drugs
The Dispatch has spent the past year uncovering how PBMs operate in Ohio and the rest of the country. Here's what you need to know from our investigation.
-
Pharmacy benefit managers (PBMs) - little-known middlemen in the supply chain that gets prescription drugs from manufacturers to consumers - receive hundreds of millions from Ohio taxpayers via the state’s Medicaid program.
-
A state-sponsored study conducted after several weeks of Dispatch stories found the PBMs are charging Ohioans 3 to 6 times the normal rate - costing taxpayers an extra $150 million to $186 million a year.
-
The PBMs use “spread pricing,” meaning they get about $225 million more a year from the state than they reimburse pharmacies for drugs used by Ohio’s poor and disabled.
-
At the same time the payments to pharmacies were being cut by the PBMs, the parent company of one of them, CVS, sent out letters to pharmacy owners sympathizing with their financial woes and offering to buy them out. This occurred in several states.
-
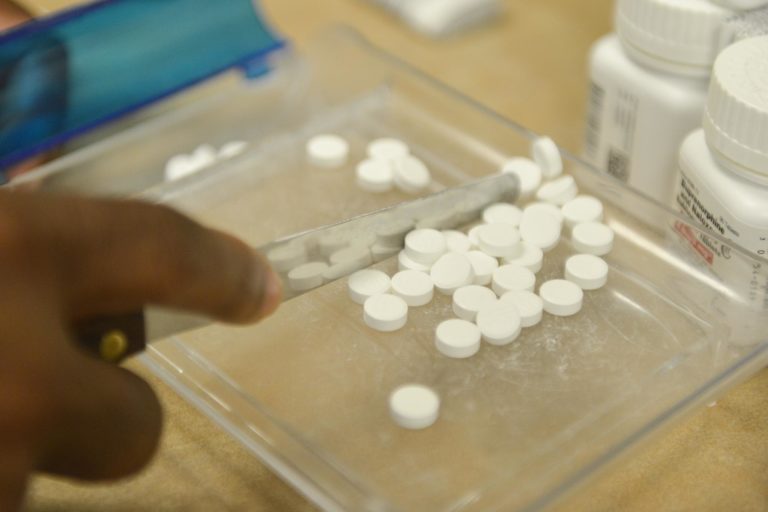
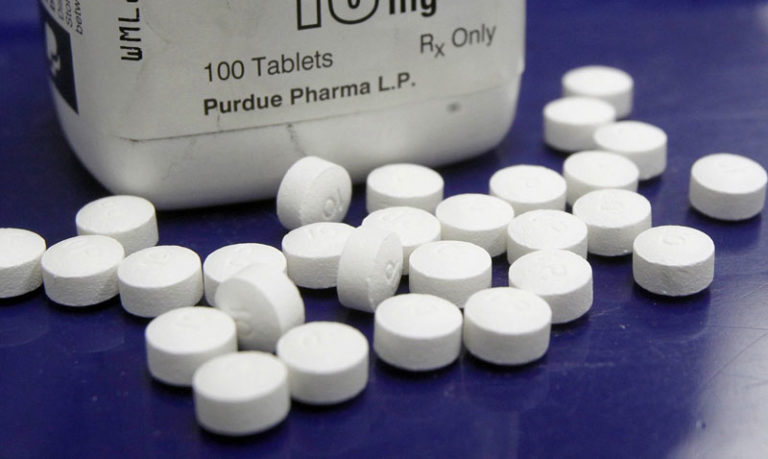
PBMs cut the reimbursement rate so much for Suboxone that many pharmacies were forced to stop stocking the drug used by numerous Ohio addicts in recovery.
-
The Medicaid official who was in charge of dealing with pharmacists who complained about low reimbursements from CVS’s PBM was at the same time, she was a part-time pharmacist with CVS Pharmacy. While still on the job at Medicaid, she negotiated a new job with CVS Caremark, the company whose reimbursements Ohio pharmacists were complaining about.
-
Ohio Medicaid officials don’t want to follow the example of West Virginia, which eliminated PBMs and saved $38 million, saying it would actually cost the Buckeye State more. Medicaid also is not following the example of the Ohio Bureau of Workers’ Compensation revamp of its prescription drug setup, with one BWC official saying “we were being hosed” under the previous deal.
-
The city of Columbus wound up doling out $8,000 a prescription for a pain cream that drug salespeople marketed as “free” to individual members of safety forces.
-
People diagnosed with cancer sometimes must wait weeks to get medication because PBMs required it to be provided by their company’s own mail-order facility, instead of having the patient get it down the hall in the same facility where they were diagnosed.
-
Rebates drive up the cost of prescription drugs, although their exact impact is cloaked.
-
A state proposal to provide HIV drugs seems to have been written so that only CVS could get it
-
The proposed merger between CVS and health-insurance giant Aetna would further consolidate the health-care market and, analysts say, drive up prices for consumers.
Report finds that drug rebates drive up consumer costs
Feb. 11, 2020
Discounts by pharmaceutical manufacturers to drug middlemen appear to be driving up list prices and ultimately some consumer costs, a new report by a team of researchers at the University of Southern California says.
The phenomenon appears to be another symptom of an uncompetitive marketplace, they said.
“It could force clinics to close their doors...” Lawmakers take aim at pharmacy middlemen
Jan. 28, 2020
Bipartisan legislation would prohibit PBMs from redirecting savings from discount drug program intended to benefit the poor.
Drug middleman fires back in workers’ comp suit
Jan. 8, 2020
Pharmacy benefit manager OptumRx says a state agency “unilaterally” made new rules in the middle of a negotiation. They were made to enact laws passed by the legislature.
Despite promised Medicaid reforms, Ohio pharmacists skeptical about 2020
Dec. 31, 2019
Ohio pharmacists are saying that a new deal offered through the state’s largest Medicaid managed-care provider appears to be marginally better than the one that preceded it. But they say too many variables and a continuing lack of transparency leave them dubious about their prospects for the new year.
AWP: Three little letters that could affect your wallet and health
Dec. 22, 2019
If you have health insurance — from your employer, your union, workers’ comp, Medicaid or Medicare — the price you’re paying almost certainly is based on a formula that relies in part on an “average wholesale price” for prescription drugs.
And it’s just as arbitrary and meaningless as the AWP for that fictional new car.
Pharmacy benefit manager OptumRx overcharged Ohio BWC by millions, Yost says
Nov. 25, 2019
In the state’s most aggressive action yet against controversial middlemen in the drug-supply chain, Attorney General Dave Yost upped the ante in a multimillion-dollar lawsuit against the pharmacy benefit manager handling prescription costs for Ohio workers injured on the job.
After months of mediation with OptumRx failed to resolve the legal dispute, Yost’s office filed an updated complaint Friday saying the Texas-based PBM “overcharged millions” by levying excessive costs for drugs prescribed through the Ohio Bureau of Workers’ Compensation. OptumRx breached its contract by not living up to its obligation to give the state the best available rate, Yost’s office says.
Ohio Medicaid still “hemorrhaging” money to pharmacy middlemen, expert testifies
Nov. 21, 2019
A national drug-pricing consultant says that despite implementing a new pricing system and other efforts to rein in pharmacy middlemen, Ohio’s Medicaid program continues “hemorrhaging” tax dollars.
“You are hemorrhaging money right now,” Linda Cahn, a critic of pharmacy benefit managers, or PBMs, told the Joint Medicaid Oversight Commission on Thursday.
Walgreens buys and shuts small chain, continuing to shrink Ohio options
Nov. 14, 2019
Pharmacy options for Ohioans — particularly those using the state's largest Medicaid managed-care provider — continue to shrink.
Walgreens confirmed Friday that the chain recently bought seven community pharmacies and then closed them about two weeks ago. The company closed another recently purchased store in Indianapolis. Walgreens moved customers' prescriptions to its own stores, which in some instances were nearby. In others, not so much.
Ohio Medicaid taking greater control of prescription drug coverage
Nov. 8, 2019
Making good on a promise to keep a closer watch on pharmacy middlemen and drug prices in Ohio’s $28 billion health-care program for the poor and disabled, state Medicaid officials unveiled a single list of medications Friday it will cover without prior authorization for all beneficiaries.
Ohio lawmaker proposes sweeping restrictions on pharmacy middlemen
Nov. 8, 2019
Dissatisfied with state efforts to rein in pharmacy middlemen, an Ohio lawmaker has introduced sweeping legislation aimed at controlling prescription drug prices.
Ohio's largest Medicaid provider cuts ties with Walgreens
Oct. 25, 2019
Walgreens, Ohio’s second-largest pharmacy retailer, will exit Ohio’s largest Medicaid pharmacy network as of Jan. 1.
Dispatch analysis shows "cost cutting" middlemen reap millions
Ohio experience raises questions about CVS-Aetna merger
Ohio firing pharmacy middlemen that cost taxpayers millions
Amid PBM inquiry, officials' ties to CVS questioned
Pharmacy middlemen come between cancer patients and their drugs
CVS accused of using Medicaid business to drive out retail competition
Ohio getting a better deal from PBMs, but many questions remain
Sept. 30, 2019
Medicaid Director Maureen Corcoran said Ohio is getting a better deal on prescription drugs since switching to a new drug-pricing system designed to rein in pharmacy middlemen.
U.S. military community beset by pharmacy-middleman headaches
Sept. 28, 2019
Millions of U.S. service members and veterans are among a group that some say is being ill-served by one of the three huge pharmacy middlemen that dominate America’s drug marketplace.
Ohio’s pharmacy benefit managers back in spotlight of Medicaid-oversight panel
Sept. 16, 2019
The legislative committee that oversees Ohio’s $28 billion Medicaid program will meet Thursday for the first time this year, and legislators want to know whether the state has made progress in addressing long-standing concerns about pharmacy middlemen profiting off prescription drugs for the poor and disabled.
Specialty drug prices leap in Ohio, lifting bottom line for pharmacy benefit managers
Sept. 7, 2019
When the big ball slowly dropped in Times Square to mark the dawn of 2019, something much less visible happened about 500 miles away: The price tag of specialty drugs for Ohio’s neediest residents suddenly jumped.
A prescription for 90 tablets of Capecitabine, a chemotherapy drug, cost about $1,175 on Dec. 31, 2018. That eye-opening price looked downright cheap next to the one on Jan. 1, 2019: more than $2,000, a 70% increase.
Specialty drug prices leap in Ohio, lifting bottom line for pharmacy benefit managers
Sept. 7, 2019
When the big ball slowly dropped in Times Square to mark the dawn of 2019, something much less visible happened about 500 miles away: The price tag of specialty drugs for Ohio’s neediest residents suddenly jumped.
A prescription for 90 tablets of Capecitabine, a chemotherapy drug, cost about $1,175 on Dec. 31, 2018. That eye-opening price looked downright cheap next to the one on Jan. 1, 2019: more than $2,000, a 70% increase.
Pharmacy middleman secrecy trial delayed again
Aug. 1, 2019
Franklin County Common Pleas Judge Jenifer French granted another delay in a trial over whether two pharmacy middlemen can keep secret portions of a report showing that the companies billed taxpayers hundreds of millions more for prescription drugs than they paid pharmacists for them.
The delay moves the trial date to March 9, 2020, meaning that at the earliest, the case will be heard 20 months after it was filed.
DeWine’s vetoes on pharmacy benefit manager revamp get mixed reviews
July 18, 2019
Many of Gov. Mike DeWine’s 25 budget vetoes had to do with sweeping reforms to the pharmacy middlemen serving the state’s Medicaid system, but the governor insisted that he remained committed to efforts to overhaul the costly setup blamed for gouging both Ohio pharmacies and taxpayers.
Still, DeWine’s actions were greeted with a mixed reception Thursday.
Ohio’s budget deal would dump current PBMs, give pharmacists $100 million
July 16, 2019
Ohio House and Senate leaders have agreed on a plan to add transparency and give the state unprecedented control over of Medicaid pharmacy benefits while slashing the authority of private managed care companies and the pharmacy middlemen they hire.
Pharmacy benefit managers poised to grab money they've already paid to Ohio pharmacists
July 14, 2019
Struggling Ohio pharmacists have been encouraged in recent months that one of two companies that determine their Medicaid reimbursements has been paying a little better for prescription drugs since the issue blew up last year.
But numerous pharmacists — and the drug-buying groups that represent them — fear that middlemen OptumRx and CVS Caremark will both take a big chunk of their money back in the coming months.
Dispute over reining in drug middlemen key in Ohio budget impasse
July 8, 2019
A key holdup in Ohio’s state budget stalemate centers on how to deal with pharmacy benefit managers.
The middlemen in the Medicaid drug supply chain were targeted by both branches of the legislature. But House and Senate members remain far apart on what they see as a solution.
Pharmacy 'deserts' appear in Ohio as stores close amid drug pricing debate
July 7, 2019
DANVILLE, Ohio — Maintaining access to the kinds of care that keep people out of the emergency room is becoming more difficult in the sparsely populated corners of the Buckeye State. Some say big corporations that work with the Ohio Medicaid program are partly to blame.
Small town pharmacy prospers in other states, suffers in Ohio
June 23, 2019
WELLSTON, Ohio — It's been more than a year since state officials declared they were going to bring sunlight and fairness to Ohio's Medicaid drug-reimbursement system.
Senate budget strips PBM changes sought by House
June 12, 2019
Majority Republicans in the Ohio Senate on Wednesday stripped from the House-passed budget provisions that would give the state more control of private pharmacy benefit managers in the Medicaid program.
State, former pharmacy benefit manager seek to settle legal dispute over drug costs
June 12, 2019
The Ohio Bureau of Workers’ Compensation and its former pharmacy benefits manager, OptumRx, will try to resolve a $16 million legal dispute through confidential, non-binding mediation.
Senate budget strips PBM changes sought by House
June 12, 2019
Majority Republicans in the Ohio Senate on Wednesday stripped from the House-passed budget provisions that would give the state more control of private pharmacy benefit managers in the Medicaid program.
Drug middlemen name own prices, methodology goes unchallenged
June 10, 2019
Ohio Medicaid officials and their managed-care contractors say they're bringing new transparency to an opaque drug-delivery system that in 2017 saw more than a quarter-billion-dollar markup to taxpayers. But none of them will address a system under which the middlemen get to decide what drug prices are.
Pharmacy benefit managers again take center stage in CVS-Aetna case
June 5, 2019
CVS’ pharmacy benefit manager business once again emerged as a key concern Wednesday in a possible merger between the pharmaceutical giant and health insurer Aetna.
PBMs become potent symbol in federal court hearing over CVS-Aetna merger
June 5, 2019
U.S. District Court Judge Richard Leon was near the end of his first day in what is scheduled to be a three-day hearing on the proposed merger of CVS and Aetna when he began marveling over the power that CVS’ pharmacy benefit manager has.
New 'transparent' Medicaid pharmacy contract quickly withdrawn
June 3, 2019
Ohio's largest Medicaid managed-care provider promised unprecedented transparency earlier this year as it dropped its pharmacy middleman, CVS, and hired a new one. But until the new contract by middleman Express Scripts was abruptly pulled back last week, it bore many of the features of earlier deals that cost taxpayers more than a quarter billion dollars a year in markups and that community pharmacists said were driving them out of business.
Transparency promised on Ohio Medicaid drug prices falls far short
June 2, 2019
“Transparency” was the key word for two waves of reforms to Ohio’s pharmacy benefit managers that took effect in July 2018 and January 2019.
Federal judge wants unrestrained review of proposed $69B merger of CVS, Aetna
May 23, 2019
A federal judge had stern words for CVS, Aetna and the U.S. Justice Department as he scheduled a crucial hearing to consider whether a merger of the two companies is in the public interest.
Medicaid drug-service switch raises questions about past practices
May 20, 2019
Another of Ohio's five Medicaid managed-care plans says it is jettisoning CVS Caremark as its manager of hundreds of millions of dollars worth of pharmacy benefits.
The company, Buckeye Health Plan, is hailing the June 1 change as a move toward increased transparency. But it raises new questions about whether CVS and Buckeye owner Centene Corp. — two of the 60 largest companies in the country by revenue — have overbilled Ohio's health program for the poor.
Ohio's battle with drug costs provides road map for other states
May 15, 2019
If there is a bright side to Ohio’s misfortune with Medicaid drug costs, it would be helping other states avoid similar pricing schemes.
When federal regulators announced new guidelines this week to crack down on excessive profits by private Medicaid managed-care companies and their pharmacy benefit managers — also known as PBMs — they credited Ohio for its effort to combat the problem.
New federal regulation targets excessive profits by pharmacy benefit managers
May 15, 2019
Citing Ohio’s struggles with rising drug costs, federal regulators on Wednesday announced new reporting guidelines for tax-funded Medicaid managed-care plans aimed at eliminating excessive profits.
The Centers for Medicare and Medicaid Services' directive targets pharmacy middlemen’s use of “spread pricing” and rebates from drug manufacturers to boost earnings.
Cancer patient on PBMs: 'It's scary when you're in the hospital and they say, "denied" '
May 12, 2019
Pharmacy middlemen and the insurers they represent give themselves a lot of leeway in deciding when or whether they'll pay for expensive cancer drugs — leeway that patients and care providers say can cut lives short.
Aetna bid to derail whistleblower case against CVS denied
May 6, 2019
Insurance giant Aetna has been fighting in court to suppress records that a top company insider says show that pharmacy middleman CVS Caremark overbilled Medicare more than a billion dollars for prescription drugs.
A bipartisan Congress is moving quickly on pharmacy benefit managers
May 1, 2019
Acting with unusual speed, the U.S. House and Senate are moving forward with a pair of bipartisan bills that would require the Federal Trade Commission to investigate whether the pharmacy benefit manager industry is competitive enough.
Ohio Medicaid officials to crack down on PBM specialty drug practice
April 30, 2019
Ohio Medicaid officials are cracking down on another lucrative tactic pharmacy middlemen use to boost profits — from expensive specialty drugs.
Movement to reform pharmacy middlemen reaches a boiling point
April 29, 2019
They once were the obscure middlemen reaping billions off prescription-drug transactions as they worked behind a veil of secrecy. But a wave of reforms to the $400 billion-a-year industry of pharmacy benefit management is cresting across the United States.
Could Michigan's high drug prices flow south to Ohio?
April 29, 2019
A new study shows that pharmacy middlemen are profiting from Michigan’s Medicaid program much as they have in Ohio and several other states, and it also warns of a potentially new drug-pricing scheme.
Attorney General Dave Yost seeks reforms to rein in PBM abuses
April 22, 2019
Ohio Attorney General Dave Yost picked up the spray bottle and squirted the dirty "window" in his office. Then he grabbed a towel and scrubbed away at the grime for several seconds to reveal several human faces.
Trial in CVS-Optum secrecy case delayed - again
April 19, 2019
A trial into whether two giant pharmacy benefit managers can keep secret portions of an investigation into their pricing practices has again been delayed.
Franklin County Common Pleas Judge Jenifer French this week pushed back the trial date in a case filed by CVS Caremark against the Ohio Department of Medicaid until Nov. 4.
PBM executives blame drug manufacturers for high prescription prices
April 9, 2019
WASHINGTON — Executives of the leading pharmaceutical benefit manager companies blamed drug-makers for the high prices of prescription drugs.
The head of OptumRX accused drug companies of “anti-competitive tactics” to delay introduction of less expensive generic drugs.
CVS Caremark dumped by big Medicaid insurer
April 9, 2019
CareSource, by far Ohio's largest Medicaid managed-care provider, on Tuesday announced that it was firing CVS Caremark as its pharmacy benefit manager. The more than 1 million Medicaid clients served by Dayton-based CareSource now will have their prescriptions handled by Express Scripts, another of the nation's three dominant pharmacy benefit managers.
Ohio attorney general Dave Yost takes pharmacy benefit manager OptumRx to court
March 18, 2019
Ohio Attorney General Dave Yost is suing pharmacy middleman OptumRx to recover $16 million in overcharges to the state for prescription drugs.In a lawsuit filed in Franklin County Common Pleas Court on Friday, Yost demanded repayment after first seeking mediation in the dispute on behalf of the Bureau of Workers' Compensation, which hired OptumRx to manage pharmacy benefits for injured workers.
Court filings hint at more state action against PBMs
April 1, 2019
Court filings indicate that much more legal action is coming for the middlemen who administer drug benefits for state agencies.Ohio Attorney General Dave Yost promised as much in January as his agency investigated pharmacy benefit managers, which are businesses such as Express Scripts and CVS Caremark that contract with state agencies or their insurers to handle drug benefits.
Overcharges on generic Prilosec give Ohio taxpayers heartburn
March 10, 2019
For the past couple of years, Ohioans could buy the generic version of the heartburn treatment Prilosec off the shelf at most any drugstore for less than 60 cents a tablet — and less than 40 cents online.
At the same time, however, Ohioans were being charged $6.57 a tablet to provide large quantities of the exact same drug through the state’s Medicaid program.
Court battle rages on over pharmacy benefit manager secrets
March 10, 2019
The court battle to keep secret much of the information in a state report that is unflattering to two pharmacy middlemen continues to rage.
In a flurry of court filings during the past few weeks, lawyers for the Ohio Department of Medicaid have accused pharmacy giant CVS of burying it and its analyst with demands for irrelevant information. The filings come after OptumRx, the other large pharmacy benefit manager serving Ohio Medicaid, put people under oath — in part to ask who shared information with The Dispatch.
Drugmakers say consumers, not middlemen, should get rebates
Feb. 26, 2019
The senior executives of seven major pharmaceutical companies said they could lower drug prices if the Trump administration adopts a proposed rule that would eliminate rebates paid by the manufacturers to middlemen in the drug supply chain, primarily pharmacy benefit managers.
During a hearing before the Senate Finance Committee, Richard Gonzalez, chairman and chief executive officer of AbbVie, said while they want to see the final form of the rule, “we are supportive of taking the discount to the patient at the point of sale.”
Attorney General Dave Yost seeking $16 million repayment from pharmacy middleman OptumRx
Feb. 19, 2019
After nearly a year of investigating, Ohio is taking its first steps to recover money from pharmacy middlemen who do billions of dollars worth of business with state agencies.
Attorney General Dave Yost announced Tuesday that he is seeking repayment of nearly $16 million paid to pharmacy-benefit manager OptumRx by the Bureau of Workers' Compensation.
DeWine wants crackdown on pharmacy middlemen, managed-care groups
Feb. 1, 2019
Frustrated by the ongoing “rip-off" of Ohio taxpayers, Gov. Mike DeWine ordered a crackdown on Medicaid managed care plans and the pharmacy benefit managers they hire to oversee prescription drugs.
DeWine directed Medicaid Director Maureen Corcoran to rebid the managed care contracts and also ordered Medicaid and other state agencies to provide any pertinent data to Attorney General Dave Yost for a potential lawsuit against the pharmacy middlemen, known as PBMs.
Trump administration defends CVS merger, but ignores Ohio’s experience
Feb. 14, 2019
President Donald Trump has vowed to take on pharmacy middlemen, but his Justice Department has downplayed the concerns raised in Ohio about one of the biggest: CVS Caremark.
Lawmakers resume push for transparency, end to gag rules by pharmacy middlemen
Feb. 12, 2019
Two state legislators are moving quickly to take care of unfinished business in state efforts to crack down on the costly practices of pharmacy benefit managers.
Reps. Scott Lipps, R-Franklin, and Thomas E. West, D-Canton, have reintroduced legislation aimed at lowering prescription drug costs by increasing price transparency for both consumers and pharmacists.
Analyst: State's new drug setup still riddled with loopholes
Feb. 10, 2019
Gov. Mike DeWine is working to close loopholes that he says enabled pharmacy middlemen CVS Caremark and OptumRx to overcharge Ohio taxpayers as much as $180 million a year. But if that's to work, some experts say, he'll have to do better than the state Medicaid program did under his predecessor, John Kasich.
Trump's move on drug rebates good but may not lower prices, experts say
Feb. 5, 2019
The Trump administration's move last week to shine more light on the actions of pharmacy supply-chain middlemen was welcomed by many who have been critical of the not-so-transparent industry.
But, they warn, it's not nearly enough to fix the problem.
The proposed rule would no longer shield the middlemen, known as pharmacy benefit managers, from federal anti-kickback laws if they keep part of the rebates they obtain from drugmakers.
Pharmacy benefit manager: Who revealed information to The Dispatch?
Feb. 2, 2019
One of the companies that serves Ohio's Medicaid program is pushing hard in its fight to keep secret the details about the $280 million that it bills taxpayers for prescription drugs each year.
In a move that sparked criticism, OptumRx said it plans to ask people under oath whether they've spoken to The Dispatch, according to court papers OptumRx filed Monday.
CVS paid itself far more than some major competitors, report says
Jan. 20, 2019
CVS used its role as a pharmacy middleman for the Ohio Medicaid program to pay some of its biggest retail competitors far less than it pays its own stores, according to a section in a state report that CVS is fighting in court to keep secret.
For example, CVS would have to pay Walmart and Sam’s Club almost half again as much — 46 percent more — for generic drugs if CVS were to equal the rates it was paying its own pharmacies, according to a copy of the unredacted report for the Ohio Department of Medicaid that was obtained by The Dispatch.
Analysis: CVS makes dubious case for rebates’ impact on drug prices
Jan. 14, 2019
Health-care giant CVS says it wants to correct what it calls a “skewed” record on drug rebates. But experts and others say the story CVS is telling is the one that is skewed.
In a news release and a letter to the editor, the company said it’s a myth to say that the rebates it gets from drug manufacturers prompt those manufacturers to increase list prices. In those documents and a letter to all Ohio lawmakers, the company also has said it is returning all but 2 percent of the rebates it is collecting back to the health plans it represents.
Hearing on revealing CVS Medicaid-billing data is delayed for months
Dec. 24, 2018
Important information in a report that the Ohio Department of Medicaid commissioned this year now will remain secret well into next year.
It will remain secret past the time when the legislature will consider a budget, billions of dollars of which might go to CVS, and possibly past the time when a federal judge in Washington, D.C., will decide whether to approve CVS’s $70 billion merger with insurance giant Aetna.
'PBM busters' find employers unaware of price mark-ups by drug middlemen
Dec. 23, 2018
Kyle and Ken Fields were looking for a way to honor their father and preserve the pharmacy business he spent years building.
The brothers had heard complaints from businesses and universities in southwestern Ohio about rising prescription drug costs, so they began laying a foundation for Appro Rx — their version of a pharmacy benefit management company.
CVS/Aetna merger may test bounds of anti-trust law
Dec. 16, 2018
The $70 billion merger between health-care giants CVS and Aetna was sailing through.
That was despite the fact that venerable organizations such as the American Medical Association had raised serious concerns that the combination would sap even more competition from an already concentrated marketplace and inflate the cost of health care even more.
Little punishment from state for CVS over improper HIV mailing
Dec. 16, 2018
The Ohio Department of Health says pharmacy giant CVS mishandled patient information in 2017 when it send out a mailing to more than 4,000 participants in a drug-assistance program that had the letters “HIV” just above patients’ names, according to communication obtained by The Dispatch through an open-records request.
Ohio's prescription plan to be more transparent in 2019
Dec. 16, 2018
Ohio Medicaid will abandon its secretive prescription drug-pricing system in three weeks and move to a transparent system that for the first time will disclose exactly how billions in taxpayer dollars are being spent.
West Virginia's system possible model for cheaper Medicaid drug prices
Dec. 16, 2018
Ohio is struggling to bring transparency to the $2.5 billion its Medicaid system spends through its managed-care plans on prescription drugs each year. As it does that, one of its neighbors decided to take a drastically different path: Cut out the plan managers altogether.
Ohio leads way as states take on 'pharmacy benefit manager' middlemen
Dec. 9, 2018
Officials in states across the U.S. showed little interest for years about looking into the black box of pharmacy benefit managers, the pharmacy supply-chain middlemen who were shrouded in secrecy and also have been pouring billions of dollars worth of prescription drug rebates into state coffers.
That setup provided states with more than $20 billion in rebates last year alone, an average of $450 million for each state that uses the so-called PBMs to help manage their Medicaid programs, a three-month national survey by The Columbus Dispatch revealed. Rebates are meant to be a price concession meant to lower drug costs.
Merged CVS-Aetna won't extend transparency, competition guarantees
Dec. 4, 2018
CVS and Aetna are making promises to Georgia that they seem unwilling to make to Ohio and the rest of the country.
The Peach State in November said it would approve the merger of the two companies only if they made guarantees regarding competition and transparency. A spokesman for CVS Health last week declined to say that a merged company would make similar guarantees in other states.
Audit shows company failed to keep drug costs low for taxpayer-funded Medicaid
Oct. 21, 2018
The health insurance group that billed Ohio twice the amount of its competitors to deliver medicine to Medicaid patients also fell significantly short of its goal to keep drug costs low.
The revelation is yet another from an audit by HealthPlan Data Solutions that was commissioned by the Ohio Department of Medicaid to determine whether the state is getting fair prices on drugs.
Richard Cordray, Mike DeWine back state Medicaid reform on prescription-drug middlemen
Oct. 22, 2018
A major reform to the way the Ohio Department of Medicaid buys billions of dollars worth of prescription drugs seems likely to continue regardless of who wins the governor's race Nov. 6.
The department, under term-limited GOP Gov. John Kasich, announced in August that it would tell the state's five Medicaid managed-care plans to update their contracts with pharmacy middlemen that allowed the middlemen to charge taxpayers $224 million a year more than they were paying pharmacies for prescription drugs. The Medicaid department conducted its investigation after The Dispatch used confidential pharmacy data to conduct its own analysis that showed somewhat higher markups.
New ‘gag rule’ ban is expected to lead to saving on prescriptions
Oct. 17, 2018
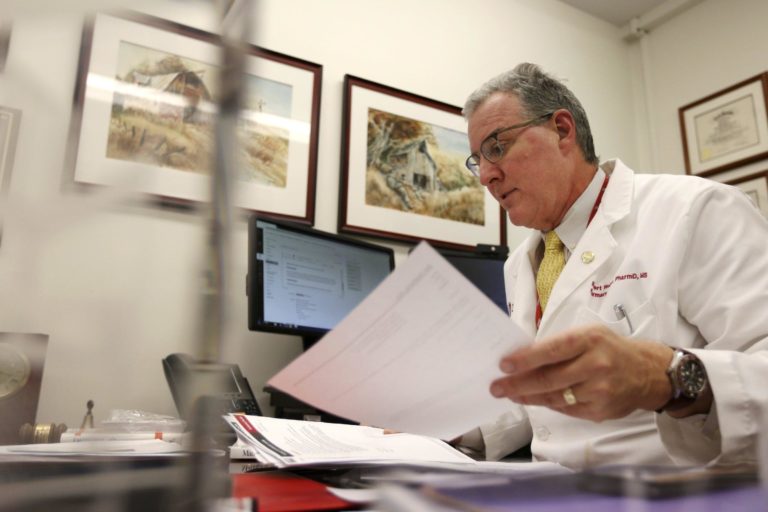
Every day, pharmacist Aaron Clark of Equitas Pharmacy in the Short North must bite his tongue and disregard what’s best for his customers.
That’s because so-called gag rules imposed by pharmacy middlemen prohibit him from telling customers how they could save money on many prescriptions by paying out of pocket instead of using their health insurance.
Ohio taxpayers may be paying twice for the same Medicaid drug services
Oct. 7, 2018
The team that discovered that Ohio taxpayers were overcharged up to $186 million for Medicaid prescription drugs last year has uncovered an additional $20 million that might have been wasted to fund services for which taxpayers already were paying.
And state Medicaid officials initially did not want that information made public.
Censored analysis confirms complaints about pharmacy benefit managers
Sept. 18, 2018
The Ohio Department of Medicaid on Tuesday released a heavily redacted report analyzing the costly practices of pharmacy middlemen in the $24 billion tax-funded Medicaid program.
The move comes as a Franklin County judge continues to mull over whether to order disclosure of the full, or unredacted, analysis of drug pricing, pharmaceutical rebates and other cost data.
State warned against pharmacy middlemen's loopholes in contract
Sept. 16, 2018
As Ohio seeks to reduce costs and bring more transparency to Medicaid’s $3 billion-plus prescription drug program, experts warn: Don’t solve one problem by creating others.
Pharmacy benefits managers, who are the middlemen in the process of pricing and paying for prescription drugs through insurance programs, are the focus of the state's attention.
Medicaid prescription transparency lauded, but Yost still has questions
August 26, 2018
The Ohio Department of Medicaid says a new plan will bring the greatest transparency in the country to its managed-care programs.
But Ohio Auditor Dave Yost — also a staunch advocate of government transparency, especially involving Medicaid — is opposed to its immediate implementation.
Ohio experience raises questions about CVS-Aetna merger
August 19, 2018
Health-care giant CVS and insurer Aetna are poised to merge into a conglomerate that would dominate three important links in the health-care chain.
It would combine the nation’s largest retail pharmacy group with the third-largest health insurer. It also would include the country’s second-largest pharmacy benefit manager — the middleman between insurers and pharmacies that extracts discounts from drug manufacturers, bills health plans and determines how much pharmacies are paid. Already the seventh-largest corporation in the United States, CVS estimates that, post-merger, it would move up a few notches on that list.
CVS says the $70 billion deal would lead to better health care for consumers by simplifying the system, increasing access, promoting better primary care and lowering costs.
Ohio Medicaid drug audit calls for transparency, highlights pharmacy closures
AUGUST 16, 2018
A state audit of Ohio's Medicaid prescription drug business says there's not nearly enough transparency for state officials to know whether taxpayers are getting their money's worth from the $2.5 billion annual expenditure.
It also raises questions about whether a reimbursement setup dominated by pharmacy giant CVS is driving smaller competitors out of business and reducing Medicaid recipients' access to medicine.
Stark pharmacies struggle amid PBM issues; CVS offered to buy stores
AUGUST 16, 2018
CANTON Ohio Auditor Dave Yost is expected to release a report this morning that should shed light on whether pharmacy benefit managers or PBMs have been overcharging the state's Medicaid program at taxpayer expense.
The report, requested by state legislators, may also provide more information on whether PBMs are inadequately reimbursing pharmacists across the state, including in Stark County, for dispensing drugs to Medicaid patients. And it could reveal the spread — the difference between what it charges Medicaid and what it pays the pharmacists for the drugs — PBMs are pocketing.
Ohio firing pharmacy middlemen that cost taxpayers millions
AUGUST 14, 2018
The Ohio Department of Medicaid is changing the way it pays for prescription drugs, giving the boot to all pharmacy middlemen because they are using "spread pricing," a practice that has cost taxpayers hundreds of millions.
Medicaid officials directed the state's five managed care plans Tuesday to terminate contracts with pharmacy benefit managers using the secretive pricing method and move to a more transparent pass-through pricing model effective Jan. 1.
How so-called rebates drive up the cost of prescription drugs
AUGUST 12, 2018
Rebates demanded by pharmacy middleman from drug manufacturers are driving up Americans' prescription-drug costs by billions of dollars.
A Dispatch analysis of financial records from the country’s largest drug manufacturers found that practices of the pharmacy benefit managers, also known as PBMs, push the list price of their drugs well beyond actual costs.
Judge rules that part of CVS/Medicaid report can be released
AUGUST 7, 2018
A Franklin County judge has blocked release of a full state report detailing the costly practices of pharmacy middlemen in the tax-funded Medicaid program - at least for now - but will allow some parts to be disclosed.
Common Pleas Judge Jenifer French Tuesday granted a temporary restraining order at the request of CVS Caremark, which argued the 51-page analysis contains trade secrets including drug pricing, rebate and cost information.
State accuses pharmacy middlemen of 'driving up costs'
July 31, 2018
For the first time, state officials flatly accused pharmacy middlemen of "driving up costs" in the tax-funded Medicaid program and hiding their activities behind a veil of secrecy.
The new accusation comes in a Franklin County court filing that fight CVS Caremark’s attempt to keep secret a $50,000 report detailing how pharmacy benefit managers charged higher-than-industry-standard costs on prescription drugs for Medicaid patients.
Was CVS favored by state in multimillion-dollar deal to provide HIV drugs?
July 29, 2018
State officials awarded a contract to CVS last year that allowed the national pharmacy company not only to control federal money for HIV drugs in Ohio, but also to require patients to buy their medicine only at CVS pharmacies
DeWine tells Ohio’s pharmacy middlemen he’s ready to sue them
July 23, 2018
Ohio Attorney General Mike DeWine is ramping up his investigation into the costly practices of pharmacy middlemen, hiring outside counsel to assist with a probe he expects to lead to litigation against companies managing drug benefits for Medicaid and other tax-funded health insurance programs.
Report on pharmacy middleman pricing to stay secret -- for now
July 17, 2018
Plans to release a report documenting the costly practices of pharmacy middlemen were shelved by Ohio Medicaid officials on Tuesday at the request of a judge reviewing claims by CVS Caremark that the analysis contains confidential information and trade secrets.
Franklin County Common Pleas Judge Jenifer French asked for the delay to allow CVS Caremark time to identify information in the 51-page report it considers proprietary and it believes should be redacted before being released to the public, lawmakers and news media.
CVS sues state to block release of report on its drug pricing
July 16, 2018
CVS Caremark is suing the Ohio Department of Medicaid to block it from releasing the full report detailing how the pharmacy middleman charged taxpayers three to six times as much to process prescription drugs for the poor and disabled as the industry standard.
"The disclosure of proprietary information in the Caremark agreements would be devastating to Caremark's entire nationwide business model," CVS attorneys argued in an 18-page request for a temporary restraining order filed Monday in Franklin County Common Pleas Court.
Local pharmacies and their personal care in danger of disappearing
July 15, 2018
Mark Kratzer's pharmacy business seems to be as much a calling as a profession.
“I’ve always told people I’ll probably die at the counter, but I don’t know if I’ll have a counter to die at,” he said at his Wilmington store, Kratzer's Hometown Pharmacy.
He's far from alone. As with other health professions, part of the attraction of pharmacy is the chance to help others, but many independent and small-chain pharmacists say that's increasingly difficult to do.
Amid pharmacy benefit manager inquiry, officials' ties to CVS questioned
Possible conflicts of interest between the Kasich administration and CVS are fueling skepticism over whether Ohioans will see changes in a Medicaid setup that gives the national pharmacy company up to six times its actual cost of providing prescription drugs to Ohio's poor and disabled.
The relationships are shrouded in secrecy — in part because of confidentiality laws and in part because the administration of Gov. John Kasich has been less than forthcoming about critical aspects of CVS’s business with the state.
The concerns are heightened because Medicaid officials withheld key information from state legislators about CVS costs and displayed a reluctance to make substantive changes to a system that many lawmakers and pharmacists say is a ripoff of taxpayers.
Lawmakers tear into Ohio Medicaid officials: Are you incompetent?
June 28, 2018
Enraged by pharmacy middlemen making millions on Ohio’s health insurance program for the poor and disabled, lawmakers tore into Medicaid officials Thursday, accusing them of withholding data, failing to recognize the scope of the problem, and ignoring recommendations for reducing costs.
"Your attitude is callous and insensitive to the poor people we all serve," said Sen. Vernon Sykes, D-Akron, as he scolded Medicaid officials before the Joint Medicaid Oversight Committee.
HIV patient sues Ohio over drug-aid program requiring use of CVS
July 5, 2018
An HIV patient is using an anti-Obamacare provision in the Ohio Constitution to sue the state for forcing him to use CVS pharmacies if he is to receive benefits under a government program that helps with drug costs.
Edward J. Hamilton of Columbus filed suit this week in the Ohio Court of Claims against the state Department of Health in connection with the department’s HIVDrug Assistance Program, which requires participants to get their medicine through the national CVS pharmacy chain.
State health department, CVS sued over HIV mailing
July 1, 2018
The Ohio Department of Health has been sued in connection with a mailing that might have publicly disclosed the identities of 6,000 HIV patients. The suit follows one in another venue against CVS Caremark, the entity that actually sent the letters.
The suit against the state says that in allowing CVS to undertake the mailing, the state was sharing patients’ private medical information without authorization.
Editorial: Ohio must demand drug-pricing transparency
July 1, 2018
The more we learn about the operations of pharmacy benefit managers, the worse their greedy scheming is revealed to be.
PBMs, as they are known, were once hailed as an answer to provide needed cost controls through claims management for insurers and payers including Medicaid. But as their middleman role between prescription-drug manufacturers and payers has grown, they have been revealed as lining their pockets on both ends of the equation.
Drug middlemen charging Ohioans triple the going rate — or more
June 27, 2018
Pharmacy middlemen are charging Ohio taxpayers three to six times as much to process prescription drugs for the poor and disabled as the industry standard.
Figures in a study commissioned by Medicaid officials indicate that pharmacy benefit manager CVS Caremark billed the state about $5.60 per script, while Optum Rx charged $6.50 per script.
CVS Caremark cut payments to pharmacies amid $70 billion deal to buy Aetna
June 24, 2018
It happened in Ohio, Arkansas, Iowa, New Jersey, New York and possibly other states. Pharmacy middleman CVS Caremark suddenly cut the reimbursements it paid community pharmacies for drugs, some of them far below pharmacists’ costs for potentially lifesaving medications.
Each of the cuts happened late last year or early this year — all within a few months of when CVS Health announced it was acquiring health insurer Aetna.
In a Dispatch review of data collected from 40 pharmacies, the numbers back up what lawmakers and critics said happened in the fourth quarter of 2017: CVS Caremark sharply reduced payments to pharmacies.
CVS Caremark hitting pharmacists with fee increase
June 22, 2018
Under increased scrutiny about millions in tax dollars it receives to manage Medicaid drug benefits, CVS Caremark announced this week it will increase the fees it charges pharmacists, including to fill prescriptions for the poor and disabled.
The transaction fee increase effective Friday came the day after a state report showed pharmacy middlemen billed taxpayer-funded Medicaid 8.8 percent more than the amount they reimbursed pharmacists.
The practice known as "spread pricing" allowed the middlemen to take a cut of $223.7 million during the year ending March 31, according to an analysis commissioned by the Ohio Department of Medicaid.
State report: Pharmacy middlemen reap millions from tax-funded Medicaid
June 21, 2018
Pharmacy middlemen managing Ohio Medicaid’s prescription drug program billed taxpayers 8.8 percent more for medications than they paid pharmacies, according to an audit commissioned by the health insurance program for the poor and disabled.
That difference — $223.7 million — was kept by CVS Caremark and Optum RX, pharmacy benefit managers for Medicaid’s five managed care plans.
The analysis of more than 39 million drug transactions for the year ending March 30 appears to be the first comprehensive review of “price spread” on behalf of a government agency, state officials said. They hope other states follow suit.
'Cost-cutting' middlemen reap millions via drug pricing, data show
June 17, 2018
A middleman company hired to keep the state's prescription-drug prices in check for Ohioans on Medicaid is receiving millions in taxpayer money meant to provide medications for the poor and disabled.
Records of transactions provided to The Dispatch from 40 pharmacies across Ohio show that CVS Caremark routinely billed the state for drugs at a far higher amount than it paid pharmacies to fill the prescriptions. The state-sanctioned practice, known as "spread pricing," allows the middlemen, called pharmacy benefit managers, to keep the difference on medications used to treat health concerns ranging from mental illness to osteoporosis.
Wary Ohio officials want deeper look at how CVS sets drug prices
June 19, 2018
Ohio’s auditor and the attorney general said Tuesday that a Dispatch investigation into a middleman that collects millions in taxpayer dollars meant for Medicaid patients has raised significant concerns and they are launching concurrent inspections.
The response is to the latest investigation by The Dispatch that found CVS Caremark billed the state roughly 12 percent more for drugs than what it paid pharmacies for medications dispensed to Ohioans on Medicaid.
'Free' pain cream costs city more than $8,000 a prescription
June 10, 2018
Armed with prescription forms and a deceptive pitch, the pharmacy reps walked into a handful of Columbus police and fire stations.
The sales line went something like this: Here is a new topical cream that will ease your aches and pains. It also will improve your skin and even help eliminate stretch marks.
The cops and firefighters were told to try it, and handed a prescription form they could give to their doctor.
"It’s of no cost to you," was how the pitch ended.
Mail-order pharmacy system delays meds for some patients
June 3, 2018
Imagine the terror of being diagnosed with cancer.
Your doctor writes a prescription that you pray will save your life. You go to the hospital or oncology clinic’s in-house pharmacy. The medicine is right there on the shelf, but you’re told the only way your insurance will cover your medication, which might cost $10,000 or more per month, is if you get it through the mail.
So, you go home empty-handed and wait. If you’re lucky, the medicine will arrive in just a couple of days. But it could be up to a month before delivery of the drugs.
Pharmacist says CVS strong-arms cancer-drug business
June 3, 2018
Josh Cox says that CVS will go pretty far in trying to wrest the lucrative business of filling cancer-drug prescriptions away from oncology clinics.
The company, which operates a retail pharmacy chain and manages prescription-drug payments for millions of Americans, has long sent unsolicited faxes to cancer doctors, using confidential patient information, in an attempt to steer business to its own pharmacies, said Cox, pharmacy director for the Dayton Physicians Network.
CVS backs away from dark-money group it contributed to
June 1, 2018
Pharmacy giant CVS Health distanced itself Friday from a pro-Trump dark-money group that it contributed to. CVS said it only learned after it made its $500,000 contribution that the group’s leaders and members have a history of racist and other kinds of hate speech.
CVS, the country’s seventh-largest corporation, said its goal in making the contribution was to advance last year’s Republican tax cut.
House committee OKs crackdown on pharmacy-benefit managers
May 22, 2018
A House committee on Tuesday recommended passage of bipartisan legislation aimed at lowering drug prices by targeting little-known middlemen in the pharmaceutical price chain.
House Bill 479, by Reps. Scott Lipps, R-Franklin, and Thomas E. West, D-Canton, would put into state law regulations on pharmacy-benefit managers, or PBMs, recently imposed by the Ohio Department of Insurance.
When pharmacy-benefit manager cuts put lives in jeopardy
May 21, 2018
Jo Anna Krohn is used to emergency calls. As director of Port 45 Recovery in Portsmouth, Krohn works with addicts in an area that is seen by some as ground zero for the nation’s opioid epidemic.
But last fall, she received a call that left her panicked.
It was from a local pharmacist warning that he could no longer stock a generic version of Suboxone because the state was reimbursing him so little for it that he was losing money.
Powerful, secretive middlemen affect drug prices
May 20, 2018
The East Side pharmacist is ready to shout out the names of his customers before they walk through the door of his spotless and brightly lit pharmacy. Typically, the medication is on the counter before the customers make their way to the register.
For an independent pharmacist, those close relationships are vital to staying in business.
But what the pharmacist can’t share with customers is the rationale behind the prices they pay for their prescription drugs.
Aetna whistleblower, who says CVS gouged Medicare and Medicaid customers, is put on leave
May 17, 2018
A whistleblower with Aetna who accused CVS Caremark of gouging Medicaid and Medicare customers with high prescription-drug costs has been placed on paid administrative leave by the insurance company.
The move comes after the whistleblower’s lawsuit was unsealed in federal court in early April. It also comes as CVS Caremark, one of the country’s largest pharmacy benefit managers, pursues the acquisition of Aetna for a reported $69 billion.
Trump targets pharmacy benefit managers, but offers few details
May 11, 2018
President Donald Trump put a big target on the backs of pharmacy middlemen that negotiate drug prices with manufacturers and set payments to pharmacies Friday as he unveiled his plan to lower prescription prices for consumers.
Trump wants to reduce the spread between the price the pharmacy benefit managers, known as PBMs, pay for drugs and rate they pay pharmacies, an opaque system critics say allows PBMs to boost their profits. The system of secret rebates and gag orders on retailers encourages manufacturers to increase prices and undermines efforts to control costs.
Medicaid pharmacy management called ‘a public embarrassment’
May 10, 2018
As an Ohio lawmaker called the state’s method of managing Medicaid pharmacy benefits “a public embarrassment,” officials at one health-care plan agreed to rework its contracts to ensure taxpayers are getting the best deal for their dollar.
It’s the first time that a plan — CareSource Ohio — publicly agreed to make changes. The system that the Ohio Department of Medicaid uses to pay most of the $3 billion it spends each year on prescription drugs has come under intense scrutiny this year.
Trump going after pharmacy-benefit managers to cut drug costs
May 9, 2018
President Donald Trump will announce sweeping new restrictions Friday on pharmacy-benefit managers — middlemen who negotiate drug prices with manufacturers and reimbursements to pharmacies — as part of a sweeping plan designed to lower Americans’ prescription drug costs.
Critics point to three companies they say are using their dominance in the $300 billion marketplace to pad their pockets and drive out competition.
Ohio workers’ comp exec on pharmacy setup: ‘We were being hosed’
May 4, 2018
As Medicaid officials investigate whether pharmacy middlemen are ripping off taxpayers by manipulating drug prices in the insurance program covering 3 million poor Ohioans, another state agency recently found it overpaid millions under a similar arrangement.
“We thought we had a solid contract that kept us from being taken advantage of (but) discovered we were being hosed,” said John Hanna, former pharmacy program manager for the Ohio Bureau of Workers’ Compensation
Ohio shies away from drug plan that saved West Virginia $38 million
May 4, 2018
West Virginia saved $38 million the first year it dumped managed care and handled pharmacy benefits for state workers and Medicaid recipients through a state university.
But Ohio refuses to even consider such a model for its multibillion-dollar Medicaid system, claiming such a change actually would cost the state money.
How can that be?
Iowa lawmaker/pharmacist literally calls ‘BS’ on CVS rationale for high drug prices
April 19, 2018
Pharmacy giant CVS has for months ignored questions in Ohio about a controversial pricing practice, but an Iowa legislative committee on Wednesday got the executive in charge to describe it.
He came after a lawmaker threatened a subpoena.
Rich Ponesse, senior director of trade finance for CVS Caremark, appeared before the Iowa House Government Oversight Committee to explain the difference between what his company pays retail pharmacies and what it charges health plans, a practice known as “spread pricing.”
Three CVS actions raise concerns for some pharmacies, consumers
April 15, 2018
First, CVS set up a website for consumers to compare drug prices.
But the site gave clear preference to CVS pharmacies, automatically putting them at the top of the comparison list. That occurred despite a “firewall” that’s legally required between the drugstore chain and CVS Caremark, the drug giant’s pharmacy benefit manager that runs the site.
Second, CVS’s benefit manager cut Medicaid reimbursements to local Ohio pharmacies this past fall, which some say put them in financial jeopardy.
CVS says it will allow state to see closely guarded drug-price list
April 7, 2018
Ohio apparently is going to get a rare look inside the “black box.”
That’s the moniker used for the closely guarded drug-price lists used by pharmacy benefit managers, which are coming under fire in the Buckeye State and elsewhere for possibly increasing taxpayers’ cost to cover Medicaid prescriptions while lowballing reimbursements to independent pharmacies.
Lawsuit: CVS pricing actions same as accused of in Ohio
April 6, 2018
Pharmacy giant CVS has billed the government far more for seniors’ drugs than it paid to retail pharmacies, an executive with insurer Aetna alleges in an ongoing federal whistleblower suit that was unsealed this week.
The executive, Aetna’s chief Medicare actuary, said CVS admitted to a practice known as “spread pricing.”
State probing whether pharmacy benefit managers are overcharging taxpayers
April 6, 2018
Ohio Medicaid officials pledged Wednesday to investigate claims that pharmacy benefit managers are paying pharmacists far less to fill prescriptions than they charge the state, allowing them to pocket the difference.
Critics say the practice, known as spread pricing, is increasing costs in the tax-funded Medicaid program and driving many pharmacies out of business because some drug reimbursements are less than the cost to pharmacies of acquiring the medication.
Millions of Ohio taxpayer dollars at stake in debate over drug prices
March 25, 2018
Pharmacy benefit managers are receiving $1.54 per pill from Ohio’s Medicaid program for a drug commonly used to treat depression.
The state pharmacy association and operators of nearly two dozen pharmacies across the state say those same pharmacy benefit managers, or PBMs, are paying them only about 18 cents for each of those pills.
Ohio Medicaid official got job with CVS while still working for state
March 22, 2018
A pharmacologist with the Ohio Department of Medicaid last year negotiated a new job with pharmacy giant CVS while she was still employed by the state. She also worked a side job for CVS for almost the entire time she worked for the state.
Ohio ethics rules require state employees involved in job talks with a business affected by their work to inform their supervisors and step back from any work that might affect the business. But on Wednesday, the employee, Margaret Scott, told The Dispatch she never made such a disclosure.
Bill targeting pharmacy benefit managers gets first hearing in Ohio House
March 20, 2018
A House committee opened hearings Tuesday on a bipartisan bill designed to lower the cost of prescription drugs.
House Bill 479 — sponsored by Reps. Scott Lipps, R-Franklin, and Thomas E. West, D-Canton — takes aim at pharmacy benefit managers, known as PBMs, and other third-party administrators that operate as a middleman between insurance and drug companies.
State lawmaker on prescription drug middlemen: ‘We’re getting hosed’
March 15, 2018
State lawmakers criticized Ohio Medicaid officials Thursday, saying they’re slow to act on complaints that private pharmacy benefit managers appear to be profiting excessively by slashing reimbursement rates paid to retail pharmacies.
“We’re getting hosed,” Rep. Mark J. Romanchuk, R-Ontario, said after he and other members of the Joint Medicaid Oversight Committee were briefed by Medicaid officials.
One month she’s supervising state drug program, next month she’s with CVS
March 16, 2018
Margaret Scott had responsibility over the Ohio Department of Medicaid’s pharmacy program until she departed last fall. Within a month, she was working for a company that is receiving billions of pharmacy dollars from Ohio’s Medicaid managed care programs.
Scott and the contractor, pharmacy giant CVS, aren’t answering questions about what happened. But the state’s ethics watchdog — while not speaking specifically about Scott’s situation — said it’s illegal for a state employee to continue to be involved in decisions that might affect an outside business while negotiating a new job with that business.
Ohio legislature will look into CVS Caremark billing practices
March 13, 2018
State officials on Wednesday are expected to announce “efforts to update” the industry that handles prescription-drug benefits for millions of Ohioans.
The news comes a day after The Dispatch reported concerns by some pharmacists that a significant player in the industry, CVS Caremark, is charging Medicaid high prices and paying pharmacies low prices for the same drugs, which they say drives out retail competition. The company denies the accusations.
CVS accused of using Medicaid rolls in Ohio to push out competition
March 12, 2018
Pharmacy giant CVS stands accused of overcharging Ohio taxpayers millions in an attempt to drive out retail competition — a charge that CVS flatly denies.
Bottom line: The company allegedly boosts its profits by overcharging insurers for medications while often reimbursing pharmacists less than the cost of the drug, critics say.
Ohio lawmakers going after pharmacy benefit managers
Jan. 25, 2018
When Ohioans go to pharmacists for their prescriptions, they generally assume they’ll be told the truth about the costs of their medicines. Some lawmakers, however, say that little-known organizations are keeping pharmacists from being honest with their clients.
Reps. Scott Lipps, R-Franklin, and Thomas West, D-Canton, say pharmacy benefit management companies (PBMs) are issuing “gag orders” to keep pharmacists quiet about what could be cheaper medicines for their clients, and keeping the extra money for themselves — something the lawmakers hope to ban with new legislation, House Bill 479.